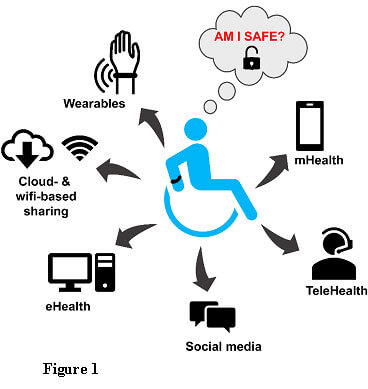
Digital preventive technologies such as mHealth, eHealth, HealthIT, and telehealth have become extremely famous among health care providers, stakeholders and patients as means of reducing healthcare costs, increase efficiency, reduce inefficiencies and errors, improve access and quality of health care and to provide personalized medical care. The use of digital preventive tools such as smart phones, computers, tablets, wearable devices, social media, and the internet have exponentially improved communications and collaborations between healthcare providers, patients, and other interested parties such as pharmacies and insurance providers. However, the greatest challenges we have faced so far include the access, management, storage and interpretation large amounts of data and health information (big data) generated by these digital prevention tools. To ensure proper data governance, data privacy, and patient security, health policies regarding digital prevention technologies are essential [1, 2]. Even though the advantages of using digital prevention tools outweigh the risks, in most cases, patients feel unsafe regarding their health data, their privacy, and security (Figure 1). Let us explore why health policy needs an update to deal with digital prevention technologies?
| Recommended for you | |
| Role of policy in digital health | |
| Convergence of preventive health care themes | |
| Preventive health care is the solution and vision for future |
5 Reasons why health policy needs an update to deal with digital prevention technologies?
1. To ensure providing equal digital services to all patients
Digital health tools while easy to use may not be adequately utilized by some of the patients who have less knowledge and exposure regarding these digital tools. For example, adults and economically-challenged patients may not be able to take full advantages of digital prevention tools. This may create a ‘digital divide’ or ‘digital discrimination’ or ‘digital inequality.’ Such digital difference may occur at different levels such as access, self-perception, usage and skills [3].
2. To ensure all digital technologies used are properly regulated
New health Apps, software, and medical devices are being developed every day. Even though they have high potential to be clinically relevant and highly useful in diagnosis and treatment, there are concerns regarding the regulations of these devices and tools. To at least partly address this challenge, the latest digital health policy that has been brought forward is ‘the 21st Century Cures Act’ in which FDA has declared a new law amending their medical software regulations to include medical devices within the Food, Drug and Cosmetic Act[4]. The Center for Devices and Radiological Health in FDA is now involved in regulation of risks and benefits of wireless medical devices, wearables, mHealth apps, medical software, cyber security and medical device data systems. As all these devices and software come under FDA’s regulation, FDA is now involved in development and implementation of new and improved health policies.
3. To ensure keeping pace of healthcare delivery with the rapidly advancing digital health technologies
The nature of digital prevention technologies is changing and adapting quickly. With these changes, many of the services are redesigned, previously manually functioned sectors are being digitized, and the infrastructure of the healthcare institutions and their partners itself are being restructured. It is critical therefore to update the health policies associated with the modifications to the technologies[5].
4. To establish regulations regarding who owns and who controls the patient data
One of the biggest concerns in the digital health world is ‘who owns patient data?’, do they belong to the patient, health institute or how much control do insurance companies have to patient data? Or are they private property or public knowledge? [6]. There have been several reports of patient personal health data breached. Therefore, some health services such as National Health Service (NHS) of England have tried to keep the patient data protected from all other parties including insurance providers, employers, advertisers, and pharmacological companies [7]. However, there has been recent debates regarding policy changes to who owns or controls patient data, where NHS is in the process of making the patient data ‘open access, ’ and insurance providers and pharmacological companies may be able to buy the patient data [8]. This is becoming an issue as in many countries, the healthcare institution owns the data, even though they may have policies regarding the retention and durability of electronic patient data [9].
5. To ensure ‘meaningful use’ of patient-generated health data (PGHD)
From wearable devices and healthcare/wellness apps, significant amounts of patient data are generated. Additionally, remote monitoring through telemedicine and mhealth provide clinically relevant yet large amounts of PGHD which may include but not limited to vital signs, allergies, symptoms, lab results, behavior, medications, life style, and habits. However, it is still of a question how this data can be used ‘meaningfully. ‘While some parties believe that PGHD should be incorporated into EHRs so that they can be utilized in the future in a meaningful manner [10], there is still unclarity regarding the reliability, validity, and usability of PGHD. As a result, currently, PGHD in Stage 3 of the EHR Incentive Programs or the Meaningful Use Program is being implemented to manage PGHD correctly[11].
Image credit: www.istockphoto.com