German healthcare system
A healthcare system is like the heart of a country. It determines the health and wellness of the country; is considered as a measurement of the development stage of a country and consumes a significant portion of the gross domestic product (GDP). A recent article written by Steve Klingaman named “Want a new health care model? The Germans do it right…” identifies the healthcare system of Germany as an example model that should be adopted by other countries as well [1].
The basic structure of German healthcare system
The basic model of the German healthcare system is a ‘universal multi-payer system’ [2] comprising of,
- Government health insurance/Statutory health insurance/public health scheme (Gesetzliche Krankenversicherung, GKV) which is used by approximately 85% of the German population.
- Private health insurance (Private Krankenversicherung, PKV) which is used by nearly 11% of the German population.
The statutory and private health insurances are also called sickness funds and (private) sickness funds, respectively. Therefore, the government of Germany and private sector are the two major players of healthcare insurance in Germany.
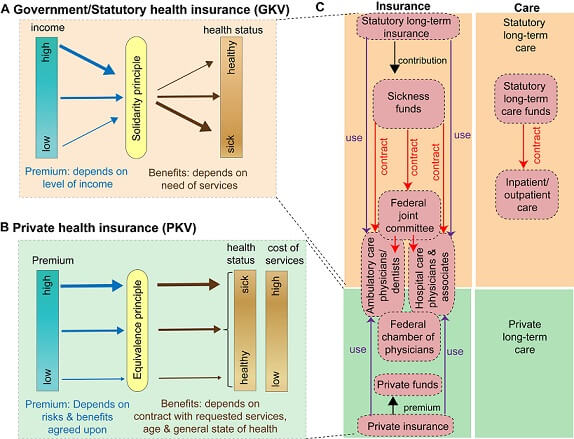
Figure 1. The basic structure of the German healthcare system. A) Government /Statutory health insurance/public health scheme (Gesetzliche Krankenversicherung, GKV). B) Private health insurance (Private Krankenversicherung, PKV). C) Organization of the German healthcare system. Panels A and B are modified from myGermanExpert blog and panel C modified from [5].
| Criteria | GKV | PKV |
|---|---|---|
| Percentage of population | ~85-90% | ~11% |
| Principle | Solidarity principle | Equivalence principle |
| Method of payment | Cost transfer | Reimbursement |
| Contribution/Premium | Depends on level of income
(14.6% of gross income) |
Depends on risks and benefits agreed upon |
| Benefits | Depends on need | Depends on contract that contains requested service, age and general state of health |
| Who is insured | Employees, artists, journalists, students, unemployed and retired people, spouses (if not working), children until a certain age | Individuals with 54,900 euros/year (as of 2015) income for at least one year, family members should be individually insured, |
Table 1. Comparison of the two major players of healthcare insurance in Germany
Ref. [2], http://blog.mygermanexpert.com/2016/05/Health-Insurance-Germany.html?m=1
Some reports suggest that the German healthcare system follows a ‘contribution-based social insurance model’ [3]. Within this model, the German healthcare system is funded and financed by the public sector. In addition to administration of sickness funds, the costs of healthcare infrastructures (such as administration, maintenance of institutions/facilities, public healthcare, and medical educations) are also taken care by the public sector. The care providers include
1) Public sector-based care providers such as government, federal, state and municipal;
2) Private institutions/providers (companies or individuals) and
3) Care providers from nonprofit organizations such as German Red Cross [4].
| Recommended for you | |
| Statutory health insurance in Germany | |
| Lobby groups in German healthcare system | |
| 20 Angel investors in Germany to finance your startup |
Self-administration & corporatism: two main features of the German healthcare system
The social insurance model of German healthcare system has five major structural characteristics [6], namely,
- Solidarity
- Benefits in kind
- Financing from employers and employees
- Self-administration
- Plurality
On the other hand, there are three governing principles of this healthcare system as well [6]. They are;
- Subsidiarity
- Self-administration
- Corporatism
Among these structural and governing principles, corporatism and self-administration are frequently mentioned in describing German healthcare system. The corporatism within the healthcare system denotes the power delegation and shifting responsibilities between different players/associations by the State [6,7]. Neither the Associations of providers nor insurance payers fully belong to public or private sectors. Legally, this is described as “corporatist associations with public obligations, and thus States have granted these organizations the power to represent and provide proper services for their consumers/patients [7]. For this reason, it is believed that the German healthcare system is a decentralized corporatist system [8].
In parallel, the States also grant significant autonomy to regulate their members within the laws and regulations of statutory healthcare insurance in Germany which is generally referred to as ‘self-administration’ (Selbstverwaltung) [7]. In the case of self-administration, ‘associations’ are the key players in this healthcare system and have more power than insurance companies or healthcare providers. Therefore, the State-granted autonomy lies within associations such as Association of statutory healthcare insurance physicians who then make contracts with insurance associations [6]. However, the State only assumes a supervisory role in this picture.
In fact, the German healthcare system follows a ‘joint self-administration’ system in between the associations of statutory health insurance and private insurance, thereby the decisions regarding budgets and patient care are made together [3].
What role do physicians play?
The physicians in German healthcare system are represented, regulated and coordinated medical associations, namely, the National Association of Statutory Health Insurance Physicians, the German Medical Association (Bundesärztekammer) and the State Chambers of Physicians (Landesärztekammer) [9,10]. The central regulatory body for doctors is the German Medical Association. These medical associations have power in governing professional policies, duties, responsibilities, decision-making processes, continued medical education, maintaining relationships and collaborations with other medical communities including research and pharmacological companies [9].
Unlike in many other countries, German physicians consider treatment of patients who have either GKV or PKV. Within each region of Germany, there are general practitioners and specialists which form regional associations that are involved in coordinating care, negotiate insurance contracts with any of the sickness funds, financial mediations between interested parties.
Many of the physicians are aided by physician’s assistants. The category of doctors includes several domains such as ambulatory care, family physicians and specialists. These physicians can either be self-employed or salaried employees of multi-speciality clinics. They provide either inpatient or outpatient care. In the case of after-hours care, German physicians are obliged to provide their services [10]. In Germany, there is no law for having a family physician, yet family physician care model is encouraged by the sickness funds [10]. It is expected that family physicians may act as gatekeepers and navigators within their healthcare system. Moreover, patients can consult specialists only by referral from a family physician [11].
Players and payers
As mentioned earlier, German healthcare utilizes a multi-payer system that has also evolved into a multi-player system. As governed by two major characteristics namely, shared decision-making powers and separate entities of GKV and PKV, there are multiple players involved in German healthcare system [10].
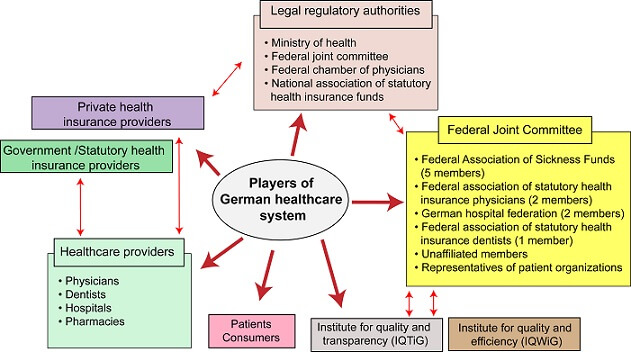
Figure 2. Multi-player nature of German healthcare system. The figure illustrates insurance payers, healthcare providers, legal, regulatory authorities and several other parties that are involved in German healthcare system.
The powers of decision-making are shared in between the federal government, states, and organizations of payers and providers which are mostly self-regulated. Under GKV and PKV, there can be a number of individual parties. Providers of statutory health insurance funds for GKV are mainly public-law corporations and companies such as BKKs, AOK, TK, SBK, and BEK [12].
There are approximately 40 private health insurance companies that German residents can choose services from.
As both insurance payers are used by the same healthcare providers, hospitals, physicians and other associations are the next layer of players in the German healthcare system [10].
Moreover, the legal regulations are set and maintained by the Ministry of Health, the Federal Joint Committee, the Federal Chamber of Physicians and the National Association of Statutory Health Insurance Physicians [12]. The Federal Joint Committee works together with the Institute for quality and efficiency (IQWiG) and the Institute for quality and transparency (IQTiG). Additionally, the Federal Association of statutory health insurance physicians and the German hospital federation collaborate with the Federal Association of sickness funds [10]. And of course, patients or consumers are major players in the German healthcare system. Last, but not least, any healthcare system is influenced by political affairs [11].
Is it a good healthcare model?
According to a recent ranking done by the World Health Organization, Germany ranks at 25th position among France, Japan, United Kingdom, Canada and USA which ranked at first, 10th, 18th, 30th and 37th [13]. Table 2 compares some of the major indicators of good healthcare systems in aforementioned countries, as a representation of the quality of German healthcare system in comparison to other nations. It is evident that Germany has either closer or above ranking of many of the healthcare system indicators compared to France which ranked 1st.
| Criteria | France | Japan | United Kingdom | Germany | Cananda | USA |
|---|---|---|---|---|---|---|
| Ranking by WHO | 1 | 10 | 18 | 25 | 30 | 37 |
| Percentage of GDP spent on healthcarea | 11.6% | 10.2% | 8.8% | 11.2% | 10.7% | 17.1% |
| Number of physicians/1000 patientsa | 3.1 | 2.29 | 2.77 | 4.05 | 2.48 | 2.56 |
| Number of acute care beds/1000 patientsa | 3.35 | 7.92 | 2.28 | 5.34 | 1.71 | 2.48 |
| EMR usea | 75% | n/a | 98% | 84% | 73% | 84% |
| Health risk factor: Obesity prevalencea | 14.5% | 3.7% | 24.9% | 23.6% | 25.8% | 35.3% |
Table 2. Comparison of healthcare system indicators in selected countries
A report written by Georg Ertl and Till Neuman based on cardiological care in Germany suggests that one of the greatest strengths of German healthcare system is the 100% comprehensive coverage of the entire population [14]. Moreover, the collaborations between the healthcare system and research studies are quite robust and German Ministry of Education and Research mediates very rapid translation of health research into clinical practice. The same article cites “Economic incentives facilitate procedures instead of comprehensive patient care” as the biggest weakness of German healthcare system [14]. Similar to any other multi-payer health care system, German healthcare system also enjoys the advantages and faces the disadvantages of a multi-payer system. The benefits include the diverse nature of the provided services for beneficiaries, cost-effectiveness, a higher rate of innovations, and is easy on the tax system. However, the less control of health expenses by the government, high administration costs and risk pools among the disadvantages of this system.
Nevertheless, given the considerable efficiency of German healthcare system, it is no wonder many other countries try to follow the footsteps of Germany [1,15,16], in order to achieve a sustainable, sophisticated and functional healthcare system.
Image credit: https://pixabay.com/de/krankenkarte-geldb%C3%B6rse-491715/
- 1. Klingaman S (2017) Want a new health care model? The Germans do it right. StarTribune.http://m.startribune.com/want-a-new-health-care-model-the-germans-do-it-right/411702466/
- 2. IQWiG_Institute_for_Quality_and_Efficiency_in_HealthCare (2015) Health care in Germany: Health insurance in Germany. PubMed Health: https://www.ncbi.nlm.nih.gov/pubmedhealth/PMH0078017/?report=reader#_PMH0078017_pubdet_.
- 3. Döring A, Paul F (2010) The German healthcare system. The EPMA Journal 1: 535-547.
- 4. Simon M (2010) Das Gesundheitssystem in Deutschland: Verlag Hans Huber Bern.
- 5. Busse R, Blümel M (2014) Germany. Health system review.: European Observatory on Health Systems and Policies.
- 6. Obermann K, Müller P, Müller H-H, Schmidt B, Glazinski B (2013) Understanding the German health care system.
- 7. Giaimo S (2016) Reforming Health Care in the United States, Germany, and South Africa: Comparative Perspectives on Health: Springer.
- 8. AOK (2012) The AOK and the German healthcare system. https://aok-bv.de/imperia/md/aokbv/aok/aokbv_info_2012_engl_311012.pdf
- 9. bundesaerztekammer About the German Medical Association. http://www.bundesaerztekammer.de/weitere-sprachen/english/german-medical-association/
- 10. Mossialos E, Wenzl M, Osborn R, Anderson C (2016) 2015 international profiles of health care systems. The Commonwealth Fund.
- 11. Sebastian Hesse, Schlette S (2012) Family physicians as gatekeepers. Health policy monitor: http://hpm.org/en/Surveys/Bertelsmann_Stiftung_-_Germany/04/Family_physicians_as_gatekeepers.html.
- 12. www.gkv-spitzenverband.de (2017) Statutory health insurance. spitzenverband.https://www.gkv-spitzenverband.de/english/statutory_health_insurance/statutory_health_insurance.jsp
- 13. WHO (2014) World Health Organization’s Ranking of the World’s Health Systems. WHO.http://thepatientfactor.com/canadian-health-care-information/world-health-organizations-ranking-of-the-worlds-health-systems/
- 14. Ertl G, Neumann T (2013) CardioPulse Survey series: Germany The strengths and limitations of the German health-care system. European Heart Journa 34: 1609–1614.
- 15. Altenstetter C (2003) Insights from health care in Germany. American journal of public health 93: 38-44.
- 16. Esmail N (2014) Lessons from Abroad A Series on Health Care Reform: Health Care Lessons from Germany. Fraser Institute.https://www.fraserinstitute.org/sites/default/files/health-care-lessons-from-germany.pdf